“You never understand life until it grows inside of you”. Pregnancy is a major event in any woman’s life. Hormonal ups and downs during the term of pregnancy lead to varied changes in the body as well as in the oral cavity. Hence, it becomes very important to maintain the pregnant woman’s current state of dental health and also preventive dental program should commence in order to deal with pregnancy related oral health issues.
The period of pregnancy is broadly in three trimesters. Implantation occurs 1 week after conception. The first trimester is the period of fetal organ formation and differentiation. This period is most susceptible to the adverse effect of the different teratogens. Therefore, care should be taken to avoid all the elective procedures and provide only the symptomatic treatment as per the needs. The second trimester marks the fetal growth and maturation. It is considered as the safest period to provide dental care. By the end of 12 weeks centre of ossification have appeared in most fetal bones, fingers and toes. Then comes the last or third trimester, and fetus continues to grow. The profound increase in the hormonal secretion, i.e., estrogen by 10 fold and progesterone by 30 fold causes several systemic as well physical changes in a pregnant lady.
Oral considerations
A detailed history about the number of times a patient had conceived or the number of abortions (if any) is an essential requirement. The appointments should be scheduled for shorter durations and the patient should be positioned in sitting up or left lateral position with the head of the dental chair elevated a little. It is best to avoid any dental radiograph during pregnancy, but if unavoidable second trimester is considered as the best and is the most preferred. Elective dental treatment is usually deferred to post partum and the drugs and evaluated and prescribed with utmost care.
Every pregnant woman should follow the preventive measures for keeping the oral environment healthy. Plaque control measures, coronal scaling, low carbohydrate intake, 2.2 mg of fluoride intake helps in reduction of Streptococcus mutans and maintaining the oral health. Any exposure to the x-ray radiations causes increased frequency of malignant disorders. It is estimated that 1 rad (equals to 0.01 Gy equals to 0.01 J/kg) of utero radiation exposure may leads to 0.1% of the malignant disorders in the newborns, sometimes causing birth of a deformed child or even death of an embryo. So in the cases of emergency requirement, proper protective measures have to undertaken in order to avoid the radiation exposure. It includes lead apron shielding, using of long cone PID (position indicating device), using proper collimation and shielding, try to avoid multiple exposures and usage of the fast helps.
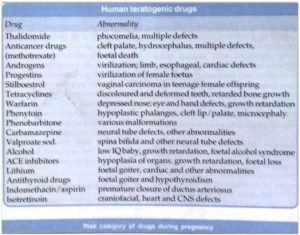
Ideally, no drug should be prescribed to a woman during her pregnancy period especially in the initial 10 weeks of gestation. But keeping in mind some of the protocols, some of the drugs can be prescribed as and when required. Always, the drug having the best safety record should be prescribed when and only definitely needed and the newer drugs should be avoided in the whole term of pregnancy. The drugs should be prescribed in intermittent dosages for short duration. Prescribing drug with lowest effective becomes important as the drug absorption slows down during pregnancy and also the drug compliance is very poor. Also, hepatic drug metabolizing enzymes are induced leading to rapid metabolic degradation. It has been seen that renal plasma flow increases by 100% and glomerular filtration rate by 70% causing rapid elimination of the drug at the time of pregnancy. The FDA (food and drug administration) has categorized the drugs according to the risk factor involved in prescribing a drug.
| Category | Drug |
| A | Controlled studies showed no risk to the patient |
| B | Either animal studies have shown no risk |
| C | Potential benefit must be greater than the risk to the fetus |
| D | Evidence of fetal risk proven |
| X | Proven fetal risk clearly outweighs any potential benefit |
FDA classification system
The safety of the drugs prescribed during pregnancy is of utmost importance. Some of the drugs used widely are classified according to their safe prescription in pregnancy.
| Drug | FDA category | Use during pregnancy | Risk | Use during lactation |
| 1.Local anaesthetics | ||||
| Lidocaine | B | Yes | – | Yes |
| Prilocaine | B | Yes | – | Yes |
| Mepivacaine | C | Use with caution; consult physician | Fetal Bradycardia | Yes |
| 2.Analgesics | ||||
| Aspirin | C/D3 | Avoid in 3rd trimester | Post partum hemorrhage; ductus arteriorus constricted | Avoid |
| Acetaminophen | B | Yes | – | Yes |
| Ibuprofen | B | Caution; avoid in second half of pregnancy | Delayed labour | Yes |
| 3.Antibiotics | ||||
| Penicillin | B | Yes | – | Yes |
| Erythromycin | B | Yes; avoid estolate form | – | Yes |
| Cephalosporin | B | Yes | – | Yes |
| Tetracycline | D | Avoid | Tooth discoloration on bone deformities | Avoid |
| Metronidazole | B | Yes | Mutagenic | Yes |
| 4.Sedatives/Hypnotics | ||||
| Barbiturates | D | Avoid | Neonatal respiratory depression | Avoid |
| Benzodiazepines | D/X | Avoid | Oral clefts | Avoid |
| 5.Corticosteroids | ||||
| Prednisone | B | Yes | Delayed labour | Yes |
Drug Administration during Pregnancy
Warfarin: It is a coumarin derivative and is contraindicated in pregnancy. It passes through the placental barrier and may cause bleeding in the fetus.
When warfarin is given during the first trimester, especially in between the sixth and ninth weeks of pregnancy, it may lead to Fetal Warfarin Syndrome (warfarin Embryopathy or Coumarin Embryopathy). It is a constellation of birth defects that includes nasal hypoplasia, depressed nasal bridge, deep groove between nostril and nasal tip, stippling of uncalcified epiphysis during the first year and mild hypoplasia of nails.

Tetracycline: It accumulates in the bone and chelates calcium which causes inhibition of bone growth and discolours the teeth.

Chloramphenicol: It falls under FDA category C and leads to bone marrow depression, irreversible aplastic anemia, agranulocytosis and most importantly Gray- Baby Syndrome. Gray baby syndrome is due to lack of glucuronidation reactions occurring in the baby, thus leading to an accumulation of toxic chloramphenicol metabolites.
Aspirin: It causes oral clefts, intrauterine death, growth retardation, pulmonary hypertension and increases the risk of antepartum and post-partum hemorrhage. Also, cyanotic heart defect leading to Blue Baby Syndrome or Tetralogy of Fallot is caused due to use of aspirin at the time of pregnancy.
Diclofenac Sodium: At maternal toxic doses, it can cause intrauterine growth retardation (IUGR). It can also decrease fetal survival chances. If this drug is used in the third trimester, it can cause constriction of ductus arteriorus with subsequent neonatal pulmonary hypertension and impaired fetal renal function.
Ibuprofen: The use of the drug can inhibit labour and prolongs the period of pregnancy. It also has a questionable association with some congenital anomalies (anencephaly, cerebral palsy, microphthalmia, nasal cleft, and tooth staining) and fetal death.
Preventive agents: Fluoride retards bacterial growth and strengthens the enamel. The Collaborative Perinatal Project (50 000 woman 12 US health centers, 1959-1974, evaluating teratogenicity of medications and drugs in first four months of pregnancy) showed no increased risk when taken during pregnancy. Xylitol gum stimulates salivation which retards bacterial growth, induces a more neutral oral pH, and assists with enamel re-mineralization. No direct studies in pregnancy have been performed, but studies where it has been used as an intervention have not demonstrated any harmful effects. Chlorhexidine has antimicrobial activity and can reduce gingivitis and plaque deposition. Vaginal application studies have shown no harm to fetus. No studies of oral use are available, but exposure would be similar when used as a rinse and spit preparation, and absorption from the gastrointestinal tract is poor.
A daily intake of 2.2 mg of sodium fluoride during the third to ninth month of pregnancy has shown to decrease caries intake in the offsprings.
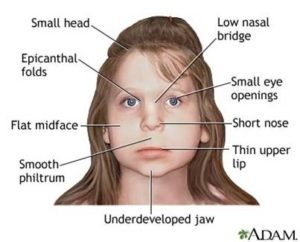
Fetal Alcohol Syndrome (FAS): It is the term given to the spectrum of the disorders that can occur as a result of alcohol consumption by the pregnant female. A cluster of cranio-facial abnormalities along with CNS dysfunction is seen in the first trimester of pregnancy. Also, pre and post natal stunting of growth is manifested in the fetus. As the child grows with advancing age, hearing, language and speech disorders are evident. The incidence rate of FAS is 0.5-1 per 1000 births in general population and mostly found in African and American population with low socio-economic status.
Smoking: Smoking by pregnant woman increases the incidence of still births, diminishes the infant birth weight and impairs the child’s subsequent mental and physical development.
Oral Complications
Poor oral care during the pregnancy leads to various of the oral diseases including pregnancy gingivitis, pregnancy granuloma, increased tooth mobility, dental caries, tooth erosion and oral candidiasis.
- Pregnancy gingivitis: It is the most common oral manifestation established due to hormonal and vascular changes occurring at the time of pregnancy. The elevated levels of circulating estrogen levels cause capillary permeability to increase which may predispose to pregnancy gingivitis. It is commonly seen in second to eighth month of pregnancy and has a tendency to bleed very easily. Scaling, root planning, curettage and oral hygiene maintenance helps to lower down the risk of pregnancy gingivitis.
- Pregnancy granuloma: It seems to occur in 5% of the women with labial interdental region of the maxillary anterior teeth as the most common site to occur. Usually, it is found to be purple to bluish in color which ulcerates and bleeds easily. The growth of the granuloma starts during the second trimester and continues to grow with an increased response of gingiva in the presence of the pregnancy hormones. It is seen to regress spontaneously after the delivery after the progesterone levels had fallen down. The larger granulomas have to be excised by the dentist.
- Oral Candidiasis: Candidiasis is often seen as a thick whitish layer on the tongue and buccal surfaces. It can be wiped off, which helps differentiate it from other oral white lesions. It is often asymptomatic, but can burn. It is more common in pregnancy because of the relatively immunocompromised state. There are other forms of oral candidiasis including angular chelitis. Treatment consists of topical and/or systemic antifungals.
- Other oral conditions related to pregnancy: Pregnant women can have either dry mouth (xerostomia) or excess saliva (ptyalism). The former can contribute to more active caries and gingivitis. Enamel erosions induced by gastric acid can occur in the patients with severe GERD or hyperemesis gravidarum.


Pregnancy Myth
“A mother looses a tooth for every pregnancy”. In reality, increased levels of estrogen and progesterone increases the circulation bringing more blood to the gingival (gums) tissues, which in turn causes swelling and increased susceptibility of the bacteria to grow in the gingival soft tissues. Teeth can loosen during pregnancy, but healthy teeth will not simply fall out. However, if a patient has pre-existing caries, gingivitis, or periodontal disease, it can worsen during pregnancy if good hygiene is not maintained and contribute to tooth loss. Women should be encouraged to brush, floss, and see a dentist for cleanings and preventive care during pregnancy.
The precise etiology of aphthous ulcers is unknown, and there is no evidence specifically linking them to pregnancy.
Changes occurring during Pregnancy that affects the oral health
Hormonal changes, mainly estrogen and progesterone, can cause a manifold changes in the mouth. The same hormones that increase ligament laxity in other joints during pregnancy can also cause increased mobility of the teeth. Severe mobility, however, may be a sign of severe periodontal disease and should be evaluated by a dentist as soon as possible. Hormonal changes can also cause changes in saliva flow, either increasing or decreasing it. Changes in the quantity and quality can also occur, making it less protective. Some types of bacteria that normally live in the oral cavity increase in numbers during pregnancy. These bacteria can cause tooth decay or gum disease.
Saliva is one of the body’s primary defenses against tooth decay. Saliva contains proteins and electrolytes that buffer and neutralize bacterial acids. It also contains the minerals calcium and phosphorus, which help to remineralize (harden) the teeth. At the time of pregnancy, buffering ability and calcium levels of the saliva are found to decrease. The bacterial count is increased in the presence low pH or more acidic saliva which causes increased tooth decay. Xerostomia or ptyalism is often experienced by a pregnant woman.
Many women experience nausea or hypoglycemia during pregnancy, which necessitates the consumption of between-meal snacks. Commonly promoted foods such as potato chips may have high content of starch (fermentable carbohydrates) that promote tooth decay. This increased frequency of food consumption and increase in carbohydrate intake can promote tooth decay by increasing the acid production of decay-causing bacteria.
Morning sickness can cause problems with oral health if the nausea makes it difficult for the pregnant woman to use a toothbrush or floss. Some women are so sensitive that they have a difficult time tolerating anything placed in the mouth.
If this causes a disruption of normal hygiene such as brushing or flossing, the bacteria that are normally present in the mouth are likely to cause pregnancy gingivitis or tooth decay.
The nausea that is often experienced during the first trimester is sometimes accompanied by vomiting. During the third trimester some women also develop severe heartburn or esophogeal reflux which propels stomach acid up into the mouth. Stomach acids irritate the gingival tissue. Stomach acids also soften the outer layers of tooth enamel allowing it to be removed easily. If this happens repeatedly the enamel will become thinned, a process called as dental erosion.
Periodontal disease and preterm labour
There is a growing body of evidence (prospective and case control studies; no randomized controlled trials) that periodontal disease is associated with an increased risk of preterm labor. The onset of new periodontal disease or activated chronic disease is caused by gram negative bacteria which may cause recurrent bacteremias and a release of lipopolysaccharide endotoxins which leads to hepatic acute inflammatory response. This in turn leads to production of cytokines and biological mediators such as prostaglandins (PGE2) and interleukins (IL-1, IL-6) as well as the systemic production of serum antibodies. These mediators can initiate labour.
Periodontal disease and low birth weight babies
As with preterm labor, animal models and human studies have demonstrated gram negative bacteria from the mouth initiating an inflammatory cascade that leads to an increase release of prostaglandins (PGE2) and interleukins (IL-1, IL-6), which in turn induce uterine contractions, placental blood flow restriction and placental necrosis with resulting intrauterine growth restriction. In some cases it may also lead to preterm labor and/or premature rupture of membranes. It is unclear which mechanism actually results in the low birth weight. Each study has controlled for confounding risks for low birth weight. However, many studies have looked at preterm labor and low birth weight concurrently which may affect outcomes.
Periodontal disease and Pre-eclampsia
Less definitive data exists for the relationship between periodontal disease and preeclampsia. Small studies point to the inflammation cascade as the culprit which causes vascular damage and placenta cell death thus initiating the same pathophysiologic responses that are proposed for any woman who develops preeclampsia. Interventions to prevent preeclampsia in women with periodontal disease have not been studied.
Obstetrical Emergencies in Dental Office
Syncope, morning sickness, seizure, bleeding and cramping are few of the emergency situations that are faced by a dentist while treating a pregnant woman.
Syncope can arise in any of the three trimesters. It can be revived by providing enough of oxygen supply, checking the vital signs and making the patient drink lots of water. The incidence of seizures is commonly present in women who are under 20 years of age, older than 35 and first-time pregnancy, are associated with chronic hypertensive pregnancy, obese pregnancy or multiple gestation events.
Pregnancy is a special event in a women’s life & hence it is an emotionally charged one………so establishing a good PATIENT-DENTIST RELATIONSHIP that encourage OPENNESS, HONESTY & TRUST is an integral part of successful management.





